Acquired gender: see Recognised Gender below. A legal/bureaucractic term used to distinguish between the gender someone was assigned at birth and the gender they feel themselves to be. Not widely used in the trans* community because of its implication that a trans* person “acquires” their gender, rather than has always been of that gender.
Assigned gender: see Acquired Gender above. Again, not widely used in the trans* community because of its implication that a trans* person can have their gender “assigned” to them by a third party, rather than has always been of that gender.
Androgynous: the gender expression of a person who has both masculine and feminine characteristics.
Bigender: a person who tends to flexibly shift between the gender behaviour typically associated with men and women depending on context.
Cis or cisgender: a person whose gender conforms to their birth sex, i.e. a male who identifies as a man or a female who identifies as a woman. The opposite of transgender.
Drag (queen or king): this refers to an actor or actress who dresses as the opposite sex for the purposes of entertainment. Not related to being trans*.
FtM or F2M: see Transman below.
Gender dysphoria: the medical term for the feeling that a trans* person has that their biological sex is not aligned with their gender identity.
Gender expression or presentation: the gender that a person appears to other people to be, selected from a spectrum of genders.
Gender identity: the gender that a person feels themselves to be, selected from a spectrum of genders.
Genderqueer: anyone with a gender identity that is non-binary, i.e. not man or woman. Genderqueer people may identify as one or more of the following: having an overlap of, or indefinite lines between, gender identity and sexual and romantic orientation; two or more genders (bigender, trigender, pangender); without a gender (nongendered, genderless, agender, neutrois); moving between genders or with a fluctuating gender identity (genderfluid); third gender or other-gendered. It also includes those who do not place a name to their gender.
Gender recognition certificate or GRC: a document certifying that for all purposes a transgender person is to be treated as the gender they feel themselves to be. In the UK, the document enables a transgender person to amend their birth certificate if they so choose.
Gender variance: a term for the feeling that a trans* person has that their biological sex is not aligned with their gender identity.
 MtF or M2F: see Transwoman below.
MtF or M2F: see Transwoman below.
Passing: the act of successfully being accepted by society as the gender that you wish to present.
Pronouns: he/him/his/his, she/her/her/hers, they/them/their/theirs. There are a range of gender neutral pronouns that have been suggested over the years. A list can be found here. Never ever use “it” when referring to a trans* person.
Recognised gender: An acceptable term used to distinguish between the gender someone was assigned at birth and the gender they feel themselves to be. The term acknowledges not only the trans person’s recognition of their “true” gender but also society’s recognition of their gender.
Sex: the biological or chromosomal sex of a person, as distinct from their gender identity or expression.
Sex-change: out-dated and unacceptable now.
She-male: unacceptable description of a transwoman.
Stealth: the condition whereby a trans* individual passes so completely that they elect not to reveal they are trans*.
Tranny: unacceptable shortened form of the word transgender or transsexual.
Trans: an acceptable shortened form of the word transgender or transsexual.
Trans*: this has replaced trans in recent years. It has been adopted by the trans* community to encompass more groups than just transsexual and transgender individuals. Trans* encompasses anyone whose gender is non-binary or fluid, i.e. androgynous, bigender, genderqueer and some intersex people.
Transgender: a term that describes someone whose gender identity is not aligned with their biological/chromosomal sex. Transgender should never be used as a noun (“I met a transgender today”). Transgender is an adjective (“I met a transgender person today”). Transgendered is also not correct (“I met a transgendered person today”) and should be avoided.
Transsexual: a term that used to be used to distinguish between someone who had undergone gender reassignment surgery and someone who had not (who would have been referred to as transgender). This has fallen out of favour as people have begun to emphasise the plurality of gender rather than accepting it as binary.
Transition: the process that a transgender person undertakes to move from being accepted as one gender to being accepted as the gender they feel themselves to be. It usually includes hormone therapy to make physical changes to the body but may or may not involve surgical procedures.
Transman: a transgender person born female but living as a man. Synonymous with the term FtM (female to male).
Transwoman: a transgender person born male but living as a woman. Synonymous with the term MtF (male to female).
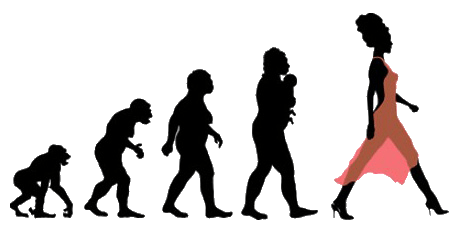
 So, to recap: Sex is biological – male or female Gender is psychological – man or woman Presentation or expression is an external representation of sex and/or gender – masculine or feminine Gender is how you would like to be perceived but, crucially, it is also how society receives your expression of that.
So, to recap: Sex is biological – male or female Gender is psychological – man or woman Presentation or expression is an external representation of sex and/or gender – masculine or feminine Gender is how you would like to be perceived but, crucially, it is also how society receives your expression of that.